Cardiac muscles are a crucial component of the human heart, playing an essential role in maintaining our overall health and well-being. Unlike other muscle types in the body, cardiac muscles are uniquely designed to handle the continuous and rhythmic contractions required to pump blood throughout the body. These specialized muscles ensure that our hearts beat consistently, providing the necessary oxygen and nutrients to our organs and tissues.
Understanding the structure and function of cardiac muscles is vital for anyone interested in cardiovascular health. These muscles are involuntary, meaning they work without conscious effort, and are characterized by their striated appearance and intercalated discs, which enable synchronized contractions. This synchronization is critical for the efficient functioning of the heart, allowing it to act as a powerful pump.
In this blog post, we will delve into the fascinating world of cardiac muscles, exploring their anatomy, physiology, and the vital roles they play in our bodies. We’ll also discuss common disorders affecting cardiac muscles and offer tips for maintaining their health. By the end of this post, you’ll have a comprehensive understanding of cardiac muscles and their importance in sustaining life.
This website may contain affiliate links. If you make a purchase through these links, I may earn a commission at no extra cost to you. Thank you for supporting this site.
Table of Contents
What are Cardiac Muscles?
Cardiac muscles, also known as myocardium, are a specialized type of muscle found only in the heart. These muscles are responsible for the continuous pumping action that circulates blood throughout the body, ensuring that oxygen and nutrients reach all cells while waste products are removed.
Definition of Cardiac Muscles
Cardiac muscles are unique in their structure and function. They are involuntary muscles, meaning they contract without conscious control, unlike skeletal muscles which are under voluntary control. This involuntary nature is crucial for maintaining a constant heartbeat, which is essential for life.
Unique Properties
Cardiac muscles possess several distinctive characteristics:
- Striated Appearance: Like skeletal muscles, cardiac muscles have a striated appearance due to the arrangement of actin and myosin filaments. These striations are visible under a microscope and indicate the organized, repetitive structure necessary for contraction.
- Intercalated Discs: One of the most unique features of cardiac muscles is the presence of intercalated discs. These specialized junctions connect individual cardiac muscle cells, allowing them to function as a single coordinated unit. Intercalated discs contain gap junctions and desmosomes, which facilitate rapid electrical communication and mechanical stability between cells.
- Involuntary Control: Cardiac muscles operate under the control of the autonomic nervous system. This ensures that the heart beats rhythmically and adapts to the body’s needs without requiring conscious effort.
Comparison with Other Muscle Types
Cardiac muscles differ significantly from skeletal and smooth muscles:
- Skeletal Muscles: These muscles are attached to bones and are responsible for voluntary movements. They are also striated but do not have intercalated discs.
- Smooth Muscles: Found in the walls of internal organs such as the intestines and blood vessels, smooth muscles are not striated and operate involuntarily, like cardiac muscles. However, they lack the complex structural organization seen in cardiac muscles.
Understanding these unique properties helps highlight the specialized role of cardiac muscles in maintaining heart function and overall cardiovascular health. In the following sections, we will explore the anatomy and physiology of cardiac muscles in greater detail, providing a comprehensive overview of their essential functions.
Anatomy and Structure of Cardiac Muscles
Cardiac muscles, integral to the heart’s function, possess a complex and unique anatomy that enables them to perform their vital role efficiently. Understanding the structure of these muscles provides insight into how they support the continuous, rhythmic contractions necessary for life.
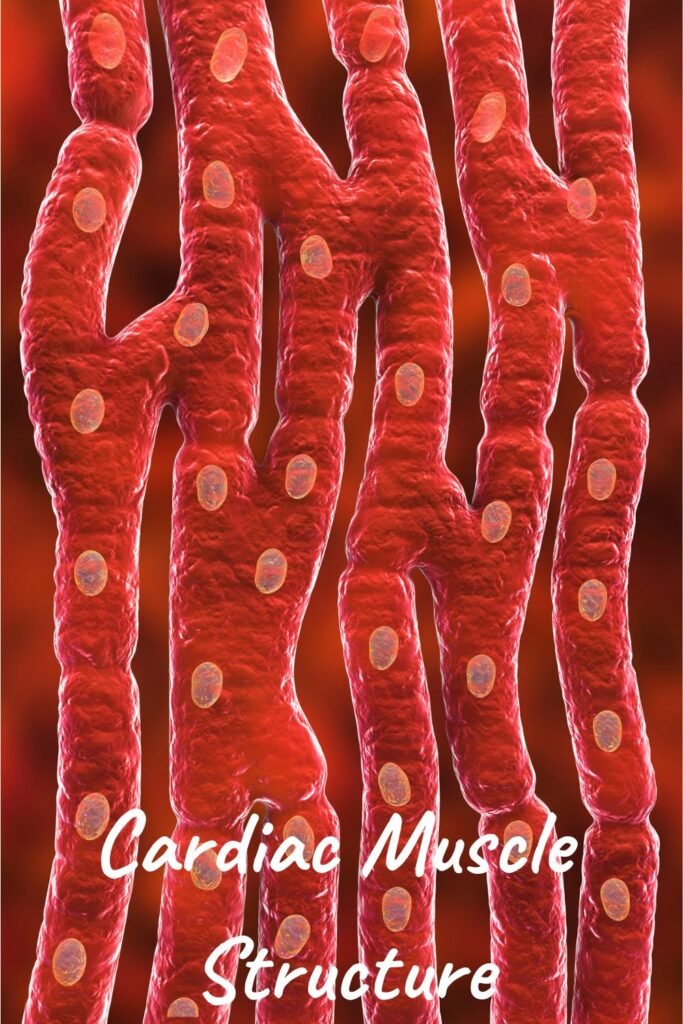
Cellular Composition
Cardiac muscles are composed of individual muscle cells called cardiomyocytes. These cells are elongated and branched, creating a network that facilitates coordinated contractions. Each cardiomyocyte contains one or two centrally located nuclei, distinguishing them from the multinucleated cells of skeletal muscles.
Striated Appearance
Cardiac muscle cells have a striated appearance due to the presence of sarcomeres, the basic functional units of muscle fibers. Sarcomeres are composed of alternating bands of actin and myosin filaments, which slide past each other during muscle contraction. This organized arrangement gives cardiac muscles their characteristic striped look under a microscope.
Intercalated Discs
One of the most distinctive features of cardiac muscles is the presence of intercalated discs. These specialized structures are junctions between individual cardiomyocytes that play a crucial role in maintaining the heart’s structural integrity and function. Intercalated discs contain three main components:
- Gap Junctions: These channels allow ions and small molecules to pass directly from one cell to another, facilitating rapid electrical communication. This ensures that the heart muscle contracts in a synchronized manner.
- Desmosomes: These structures act as mechanical anchors, holding adjacent cells together and preventing them from pulling apart during contraction.
- Fascia Adherens: These anchoring sites connect actin filaments of the sarcomere to the cell membrane, providing additional mechanical stability.
Role of Mitochondria
Cardiac muscle cells are densely packed with mitochondria, the energy-producing organelles of the cell. This high mitochondrial content is essential because the heart requires a constant and substantial supply of ATP (adenosine triphosphate) to sustain its continuous contractions. The abundance of mitochondria ensures that cardiac muscles have the energy needed to function effectively, even under varying physiological conditions.
Blood Supply
The coronary arteries provide a rich blood supply to the cardiac muscles, delivering oxygen and nutrients necessary for their function. Efficient blood flow through these arteries is crucial, as any obstruction can lead to ischemia (reduced blood flow) and potentially damage the heart muscle, resulting in conditions such as angina or myocardial infarction (heart attack).
Connective Tissue
Cardiac muscles are surrounded by a network of connective tissue that supports and protects the heart. This connective tissue matrix also helps to transmit the force generated by contracting muscle cells to the heart’s chambers, aiding in efficient blood pumping.
The intricate anatomy and structure of cardiac muscles highlight their specialized nature and essential role in the cardiovascular system. Understanding these aspects provides a foundation for exploring their functions and the physiological processes that keep our hearts beating. In the next section, we will delve into the functions of cardiac muscles and their significance in maintaining overall health.
Function of Cardiac Muscles
Cardiac muscles play a vital role in the cardiovascular system, ensuring that the heart functions efficiently as a pump. Their unique properties and highly organized structure enable them to perform several critical functions necessary for sustaining life.
Mechanism of Contraction and Relaxation
Cardiac muscles contract and relax in a highly coordinated manner to pump blood throughout the body. This process is driven by the sliding filament mechanism, where actin and myosin filaments within the sarcomeres slide past each other. This interaction shortens the muscle fibers, generating the force needed for contraction. Following contraction, the muscle fibers relax, allowing the heart chambers to refill with blood.
Coordination of Heartbeats
The heart’s ability to contract in a synchronized manner is crucial for effective blood pumping. This coordination is achieved through the heart’s electrical conduction system, which includes the sinoatrial (SA) node, atrioventricular (AV) node, and Purkinje fibers. The SA node, often referred to as the heart’s natural pacemaker, initiates electrical impulses that spread across the atria, causing them to contract. The impulse then travels to the AV node and through the Purkinje fibers, leading to the contraction of the ventricles. This orderly sequence ensures that the heartbeats rhythmically and efficiently.
Impact on Blood Circulation
Cardiac muscles are essential for maintaining proper blood circulation. The heart’s pumping action, driven by the contraction of cardiac muscles, ensures that oxygen-rich blood is delivered to the body’s tissues and organs while carbon dioxide and other waste products are carried away. The right side of the heart pumps deoxygenated blood to the lungs for oxygenation, while the left side pumps oxygenated blood to the rest of the body. This dual circulation system is vital for sustaining cellular function and overall health.
Adaptability to Physiological Changes
Cardiac muscles are highly adaptable, allowing the heart to respond to varying physiological demands. For instance, during physical activity or stress, the autonomic nervous system increases the heart rate and the force of contraction to meet the body’s increased oxygen and nutrient requirements. Conversely, during rest, the heart rate and force of contraction decrease, conserving energy. This adaptability is crucial for maintaining homeostasis and supporting diverse bodily functions.
Endurance and Resistance to Fatigue
Unlike skeletal muscles, which can become fatigued after prolonged activity, cardiac muscles are designed for endurance. Their high mitochondrial content ensures a continuous supply of ATP, enabling the heart to sustain prolonged and repetitive contractions without fatigue. This endurance is essential for the heart’s ability to function continuously throughout a person’s life.
Regulation by the Autonomic Nervous System
The autonomic nervous system plays a significant role in regulating cardiac muscle function. It consists of the sympathetic and parasympathetic nervous systems, which have opposing effects on the heart. The sympathetic nervous system increases heart rate and the force of contraction during stress or physical activity, while the parasympathetic nervous system slows the heart rate during rest and relaxation. This regulatory mechanism ensures that the heart can adapt to different physiological conditions efficiently.
The functions of cardiac muscles are fundamental to the cardiovascular system’s operation, ensuring that blood circulates effectively to meet the body’s needs. Understanding these functions underscores the importance of maintaining cardiac muscle health, which we will explore further in the subsequent sections on common cardiac muscle disorders and tips for maintaining heart health.
Cardiac Muscle Physiology
Cardiac muscle physiology involves the complex processes that enable cardiac muscles to function effectively, ensuring the heart’s ability to pump blood throughout the body. Understanding these physiological mechanisms provides insight into how the heart maintains its rhythmic contractions and adapts to varying demands.
Electrical Conduction System
The heart’s electrical conduction system is essential for coordinating the contraction of cardiac muscles. This system includes several key components:
- Sinoatrial (SA) Node: Located in the right atrium, the SA node acts as the heart’s natural pacemaker. It generates electrical impulses that initiate each heartbeat. These impulses cause the atria to contract, pushing blood into the ventricles.
- Atrioventricular (AV) Node: Situated between the atria and ventricles, the AV node receives the electrical impulse from the SA node and delays it slightly. This delay ensures that the atria have enough time to contract fully before the ventricles begin their contraction.
- Bundle of His and Purkinje Fibers: The electrical impulse travels from the AV node through the Bundle of His and into the Purkinje fibers, which distribute the impulse throughout the ventricles. This rapid conduction system ensures a coordinated and powerful contraction of the ventricles.
Pacemaker Cells and Their Function
Pacemaker cells, primarily located in the SA node, are specialized cardiac muscle cells responsible for generating and regulating the heart’s electrical impulses. These cells possess automaticity, meaning they can spontaneously generate electrical activity without external stimulation. This automaticity is crucial for maintaining a consistent heart rate and rhythm. Pacemaker cells are influenced by various factors, including the autonomic nervous system and hormonal signals, which adjust the heart rate in response to the body’s needs.
Autonomic Nervous System Regulation
The autonomic nervous system (ANS) plays a significant role in regulating cardiac muscle physiology. It consists of two main branches:
- Sympathetic Nervous System: This branch increases heart rate and the force of cardiac muscle contraction. During physical activity or stress, the sympathetic nervous system releases norepinephrine, which binds to receptors on cardiac muscle cells, enhancing their activity and enabling the heart to pump more blood.
- Parasympathetic Nervous System: This branch decreases heart rate and reduces the force of contraction. During rest and relaxation, the parasympathetic nervous system releases acetylcholine, which binds to receptors on cardiac muscle cells, slowing down the heart rate and conserving energy.
Calcium’s Role in Contraction
Calcium ions (Ca²⁺) play a crucial role in the contraction of cardiac muscles. The process of excitation-contraction coupling involves the following steps:
- Action Potential: An electrical impulse triggers an action potential in the cardiac muscle cell membrane.
- Calcium Influx: The action potential causes voltage-gated calcium channels to open, allowing calcium ions to enter the cell.
- Calcium Release: The influx of calcium triggers the release of additional calcium from the sarcoplasmic reticulum, a specialized intracellular storage site.
- Contraction: The increased calcium concentration in the cytoplasm binds to troponin, a regulatory protein. This binding causes a conformational change in the actin filaments, allowing myosin to attach and slide past actin, leading to muscle contraction.
- Relaxation: Calcium ions are pumped back into the sarcoplasmic reticulum and out of the cell, reducing cytoplasmic calcium levels and causing the muscle to relax.
Action Potentials in Cardiac Muscle Cells
Cardiac muscle cells have a unique action potential profile that includes several phases:
- Phase 0: Rapid depolarization due to the influx of sodium ions (Na⁺) through voltage-gated sodium channels.
- Phase 1: Initial repolarization as sodium channels close and potassium ions (K⁺) leave the cell.
- Phase 2: Plateau phase where calcium ions enter the cell through voltage-gated calcium channels, balancing the outward flow of potassium.
- Phase 3: Rapid repolarization as calcium channels close and potassium efflux continues.
- Phase 4: Resting membrane potential is restored, and the cell is ready for the next action potential.
This prolonged action potential and plateau phase prevent premature contractions and ensure that the heart has adequate time to fill with blood between beats.
Understanding cardiac muscle physiology is essential for grasping how the heart functions and adapts to the body’s needs. These physiological processes are fundamental to the heart’s ability to maintain a consistent and effective pumping action, crucial for sustaining life. In the next sections, we will explore common cardiac muscle disorders and strategies for maintaining heart health.
Common Cardiac Muscle Disorders
Cardiac muscles are vital for heart function, and any disorder affecting them can have serious implications for overall health. Understanding common cardiac muscle disorders helps in early detection, effective management, and prevention of complications.
Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle that impair its ability to pump blood effectively. There are several types of cardiomyopathy:
- Dilated Cardiomyopathy: The heart chambers become enlarged and weakened, reducing the heart’s pumping efficiency. This can result from genetic factors, infections, or chronic alcohol abuse.
- Hypertrophic Cardiomyopathy: The heart muscle thickens abnormally, making it harder for the heart to pump blood. This condition is often hereditary and can lead to obstructed blood flow and arrhythmias.
- Restrictive Cardiomyopathy: The heart muscle becomes rigid and less elastic, preventing the heart from filling properly with blood. This rare form is often caused by conditions such as amyloidosis or fibrosis.
Symptoms of cardiomyopathy include shortness of breath, fatigue, swelling in the legs, and irregular heartbeats. Treatment may involve medications, lifestyle changes, or surgical interventions like the implantation of a pacemaker or defibrillator.
Myocarditis
Myocarditis is an inflammation of the cardiac muscles, typically caused by viral infections, though it can also result from bacterial infections, autoimmune diseases, or exposure to toxins. The inflammation can impair the heart’s ability to pump blood and lead to arrhythmias.
Symptoms of myocarditis include chest pain, fatigue, shortness of breath, and rapid or irregular heartbeats. Treatment focuses on addressing the underlying cause, reducing inflammation, and managing symptoms. In severe cases, hospitalization may be required to stabilize the patient’s condition.
Heart Failure
Heart failure occurs when the heart’s ability to pump blood is compromised, leading to inadequate blood flow to meet the body’s needs. This condition often results from chronic high blood pressure, coronary artery disease, or previous heart attacks that have damaged the cardiac muscles.
Symptoms of heart failure include shortness of breath, fatigue, swollen legs and ankles, and persistent coughing or wheezing. Treatment involves lifestyle modifications, medications to manage symptoms and improve heart function, and in some cases, surgical procedures such as coronary bypass surgery or heart valve repair.
Arrhythmias
Arrhythmias are irregular heartbeats caused by problems with the heart’s electrical conduction system. These can range from harmless to life-threatening and can affect the rhythm and rate of the heartbeat.
Common types of arrhythmias include:
- Atrial Fibrillation (AFib): A rapid and irregular beating of the atria, which can lead to blood clots, stroke, and heart failure.
- Ventricular Tachycardia (VT): A fast, regular beating of the ventricles that can be life-threatening if not treated promptly.
- Bradycardia: A slower than normal heart rate, which can cause fatigue, dizziness, and fainting.
Treatment for arrhythmias may involve medications, lifestyle changes, and procedures such as cardioversion, catheter ablation, or the implantation of a pacemaker or defibrillator.
Ischemic Heart Disease
Ischemic heart disease, also known as coronary artery disease, occurs when the coronary arteries that supply blood to the cardiac muscles become narrowed or blocked by atherosclerosis (plaque buildup). This reduces blood flow to the heart muscle, leading to chest pain (angina) and increasing the risk of heart attack.
Symptoms of ischemic heart disease include chest pain, shortness of breath, and fatigue. Treatment focuses on lifestyle changes, medications to manage symptoms and prevent further plaque buildup, and surgical procedures such as angioplasty or coronary artery bypass grafting (CABG) to restore blood flow.
Understanding these common cardiac muscle disorders is crucial for recognizing symptoms early and seeking appropriate medical care. Timely intervention can significantly improve outcomes and quality of life for individuals affected by these conditions. In the next section, we will discuss tips and strategies for maintaining healthy cardiac muscles.
Maintaining Healthy Cardiac Muscles
Maintaining healthy cardiac muscles is essential for overall heart health and preventing cardiovascular diseases. By adopting a heart-healthy lifestyle, you can support the function and longevity of your cardiac muscles. Here are some key strategies to keep your heart strong and healthy.
Importance of Cardiovascular Exercise
Regular cardiovascular exercise is one of the most effective ways to maintain healthy cardiac muscles. Activities like walking, running, swimming, and cycling help strengthen the heart and improve its efficiency. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week.
Benefits of cardiovascular exercise include:
- Improved heart and lung function
- Lowered blood pressure
- Increased circulation and oxygen delivery to tissues
- Reduced risk of heart disease
Dietary Recommendations
A balanced diet plays a crucial role in maintaining cardiac muscle health. Focus on incorporating heart-healthy foods and nutrients into your diet:
- Fruits and Vegetables: Rich in vitamins, minerals, and antioxidants, fruits and vegetables help reduce inflammation and oxidative stress on cardiac muscles.
- Whole Grains: Foods like oats, brown rice, and whole wheat are high in fiber, which can lower cholesterol levels and improve heart health.
- Lean Proteins: Choose lean meats, poultry, fish, beans, and legumes to provide the necessary amino acids for muscle repair and maintenance without the added saturated fats.
- Healthy Fats: Include sources of unsaturated fats, such as avocados, nuts, seeds, and olive oil, which can help reduce bad cholesterol levels and support heart health.
- Limit Sodium and Sugar: Reducing sodium intake can help manage blood pressure, while limiting added sugars can prevent weight gain and reduce the risk of heart disease.
Regular Health Check-ups
Regular health check-ups are essential for early detection and management of potential heart issues. Schedule annual visits with your healthcare provider to monitor your heart health and discuss any concerns. Key assessments may include:
- Blood pressure measurement
- Cholesterol level checks
- Blood sugar tests
- Weight and body mass index (BMI) assessment
- Electrocardiograms (ECG) or other heart function tests if needed
Managing Stress
Chronic stress can negatively impact cardiac muscles and overall heart health. Implement stress-reducing techniques into your daily routine to help manage stress levels effectively:
- Mindfulness and Meditation: Practices like mindfulness meditation can help reduce stress and promote relaxation.
- Physical Activity: Exercise is a natural stress reliever that releases endorphins and improves mood.
- Hobbies and Social Connections: Engage in activities you enjoy and maintain strong social connections to boost emotional well-being.
Avoiding Harmful Habits
Certain habits can harm your cardiac muscles and increase the risk of heart disease. Avoiding these can significantly improve heart health:
- Smoking: Smoking damages the cardiovascular system, reduces oxygen supply to cardiac muscles, and increases the risk of heart disease. Quitting smoking can drastically improve heart health.
- Excessive Alcohol Consumption: Limit alcohol intake to moderate levels to avoid its negative effects on the heart. The American Heart Association recommends no more than one drink per day for women and two drinks per day for men.
- Sedentary Lifestyle: Avoid prolonged periods of inactivity. Incorporate movement into your daily routine, such as taking short walks, using stairs instead of elevators, and standing up regularly if you have a desk job.
Maintaining a Healthy Weight
Maintaining a healthy weight is crucial for reducing the strain on your heart and preventing conditions like hypertension, diabetes, and high cholesterol, which can affect cardiac muscles. Combine regular exercise with a balanced diet to achieve and maintain a healthy weight.
By following these strategies, you can support the health and function of your cardiac muscles, reducing the risk of heart disease and improving your overall well-being. In the next section, we will explore recent advances in cardiac muscle research and potential future developments in treatment and understanding.
Advances in Cardiac Muscle Research
Research on cardiac muscles has made significant strides in recent years, leading to a better understanding of heart function and the development of innovative treatments for cardiovascular diseases. Here are some of the most promising advances in cardiac muscle research.
Breakthrough Studies
Several breakthrough studies have shed light on the intricate workings of cardiac muscles and potential new therapies:
- Regenerative Medicine: Researchers are exploring ways to regenerate damaged cardiac muscles using stem cells. Stem cell therapy aims to repair or replace damaged heart tissue, offering hope for patients with heart failure or severe myocardial infarction.
- Gene Editing: Advances in gene editing technologies, such as CRISPR-Cas9, have opened new avenues for treating genetic heart conditions. By precisely targeting and correcting genetic mutations, scientists hope to prevent or cure inherited forms of cardiomyopathy and other cardiac disorders.
- Molecular Mechanisms: Studies on the molecular mechanisms underlying cardiac muscle function have identified new drug targets. Understanding how proteins and signaling pathways regulate heart muscle contraction and relaxation can lead to the development of more effective medications.
Emerging Therapies
New therapies are being developed to improve the treatment of cardiac muscle disorders:
- Bioengineered Heart Tissues: Scientists are creating bioengineered heart tissues using 3D printing and tissue engineering techniques. These tissues can potentially be used to repair damaged heart areas, providing a new approach to treating heart failure and other conditions.
- RNA-based Therapies: RNA-based therapies, such as antisense oligonucleotides and RNA interference, are being investigated for their potential to modulate gene expression in cardiac muscles. These therapies could offer targeted treatment options for various cardiac diseases.
- Innovative Drug Delivery Systems: New drug delivery systems, such as nanoparticles and hydrogels, are being designed to deliver medications directly to the heart. These systems aim to enhance the effectiveness of treatments while minimizing side effects.
Future Research Directions
The future of cardiac muscle research holds exciting possibilities:
- Personalized Medicine: Advances in genetic research and data analytics are paving the way for personalized medicine in cardiology. By understanding an individual’s genetic makeup, researchers can develop tailored treatments that are more effective and have fewer side effects.
- Artificial Intelligence (AI): AI and machine learning are being utilized to analyze vast amounts of data and identify patterns in cardiac health and disease. These technologies can help predict heart disease risk, optimize treatment plans, and improve patient outcomes.
- Wearable Technology: Wearable devices that monitor heart activity in real-time are becoming increasingly sophisticated. These devices can provide valuable data for researchers and help patients manage their heart health more effectively.
Collaborative Efforts
Collaborative efforts between researchers, healthcare providers, and technology companies are driving progress in cardiac muscle research:
- Global Research Networks: International research networks and collaborations are enabling the sharing of knowledge, resources, and data. These partnerships accelerate the pace of discovery and facilitate the development of new treatments.
- Public-Private Partnerships: Partnerships between academic institutions, government agencies, and private companies are fostering innovation in cardiac muscle research. These collaborations bring together diverse expertise and funding to tackle complex challenges.
Advances in cardiac muscle research are transforming our understanding of heart function and paving the way for new treatments and therapies. As researchers continue to make discoveries and develop innovative solutions, the future looks promising for improving heart health and treating cardiovascular diseases. In the next section, we will conclude with a summary of the key points discussed and reinforce the importance of cardiac muscles in overall health.
Conclusion
Cardiac muscles are fundamental to the heart’s ability to function as an efficient and reliable pump, ensuring that blood circulates throughout the body to sustain life. Understanding the anatomy, physiology, and functions of cardiac muscles provides valuable insights into how the heart maintains its vital role.
From the unique cellular composition and specialized structures like intercalated discs to the intricate mechanisms of contraction and electrical conduction, cardiac muscles are marvelously adapted for their continuous and rhythmic work. Maintaining the health of these muscles through regular exercise, a balanced diet, stress management, and avoiding harmful habits is crucial for preventing cardiovascular diseases and promoting overall well-being.
Awareness of common cardiac muscle disorders such as cardiomyopathy, myocarditis, and heart failure highlights the importance of early detection and effective management. Advances in cardiac muscle research, including regenerative medicine, gene editing, and personalized therapies, offer hope for new treatments and improved outcomes for patients with heart conditions.
As we continue to explore the complexities of cardiac muscles, collaborative efforts and innovative technologies will drive progress, paving the way for future breakthroughs in heart health. By prioritizing cardiac muscle health and staying informed about the latest research, we can contribute to a healthier and more resilient cardiovascular system.
In summary, cardiac muscles play an indispensable role in maintaining our health. By understanding their functions, recognizing potential disorders, and adopting heart-healthy practices, we can ensure that our hearts remain strong and capable of supporting us throughout our lives.
References
To ensure the accuracy and reliability of the information provided in this blog post, the following sources were consulted:
- American Heart Association (AHA): For comprehensive information on heart health, cardiovascular diseases, and recommendations for maintaining a healthy heart.
- Mayo Clinic: For detailed explanations on the anatomy, function, and disorders of cardiac muscles, as well as tips for maintaining heart health.
- National Institutes of Health (NIH): For insights into the latest research and advancements in cardiac muscle therapies and treatments.
- Harvard Medical School: For expert advice on the benefits of cardiovascular exercise and dietary recommendations for heart health.
- Centers for Disease Control and Prevention (CDC): For statistics and information on heart disease prevalence and prevention strategies.
- Journal of the American College of Cardiology (JACC): For peer-reviewed research articles on cardiac muscle physiology, pathology, and emerging treatments.
- WebMD: For accessible information on common cardiac muscle disorders, symptoms, and treatment options.
These references provide a solid foundation for understanding cardiac muscles and offer valuable insights into maintaining heart health and staying informed about the latest medical advancements.